Ideas
Long Read: Is India Prepared For Coronavirus Outbreak?
- India’s actions so far over Covid-19 spread have been satisfactory with testing capacity expanding rapidly.
- Can India pull off a miracle?
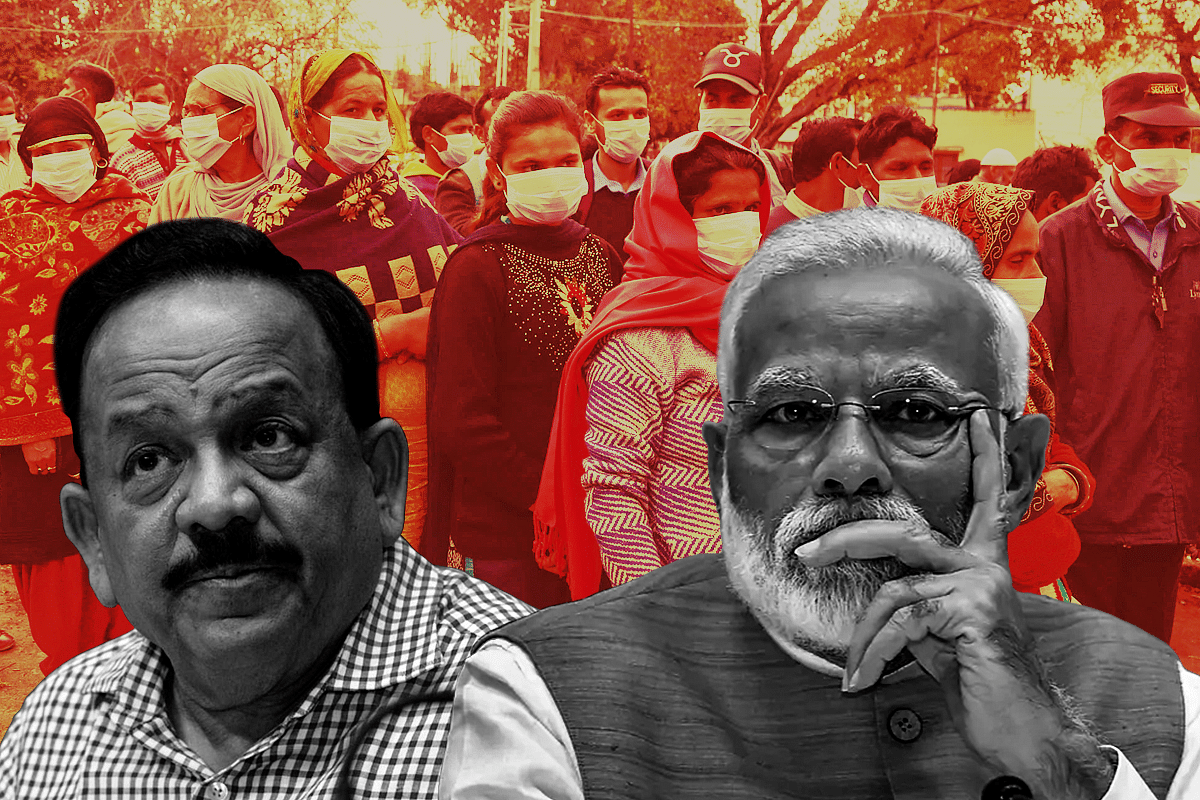
Prime Minister Narendra Modi and Health Minister Dr Harsh Vardhan
Novel Coronavirus — officially designated by the World Health Organisation (WHO) as COVID-19 — has spread to over 100 countries as of 8 March with infections crossing one lakh figure, and deaths over 3,500.
India, which had been lucky until last week to keep the virus out, is now finding itself on high alert as numbers have been rising every other day. On 2 March, the government announced that two people, one in Delhi and one in Telangana have tested positive for Covid-19. They had travel history of Italy and Dubai respectively.
As I write, the number stands at 39. Sixteen of these are Italian nationals who had come to India on a tourist visa. As it turns out, only one person in the group had Covid-19. During the course of his stay and travel in India, he managed to infect 16 of his compatriots including his wife in addition to giving it to the group’s tour driver who is an Indian.
Similarly, the Delhi patient infected six of his family members, who he visited in Agra soon after coming from abroad. The techie in Hyderabad seems to have travelled via a bus from Bengaluru to Hyderabad with tens of passengers on board. He came in contact with many of his friends and colleagues in both these cities.
Unrelated to these two cases are a couple of people in Ghaziabad and Gurgaon who tested positive on 5 March. Five fresh cases are being reported from Kerala, two from Jammu and Kashmir, one from Tamil Nadu. All have either travel history from affected countries or have been infected by their relatives who came from abroad.
The pattern should be clear from these series of fresh cases. There were clear lapses at airports in screening passengers with travel history to countries, which are seriously impacted such as Italy. The government either delayed announcing tough restrictions on passengers coming from Covid-19 hotspots or blundered in not doing screening properly.
Measures like universal screening of all passengers coming to India from anywhere and suspending visas of those with travel history from severely infected countries came too late on 3 March, when two cases were detected who may in turn have ended up infecting several others.
The paranoia and panic not shown at the country’s airports means that now the efforts required to contain the fast spreading Covid-19 cases will have to be many times more.
That’s the nature of Covid-19 sadly. The efforts the authorities need to put to contain it increases exponentially with each new case. And as other countries are finding out, if they had to do it all over again, they wish they had put a complete ban on all flights much earlier and more strictly than deal with the mess that’s at their doorsteps now.
Second Chance
The best case scenario for a nation to prevent Covid-19 spread is to keep it out of its borders by whatever means possible without thinking much about the economic costs. Because these costs are nothing compared to the losses that would follow if Covid-19 spreads.
But many countries have bungled in keeping the virus out including India. They do get a second chance but the window of action is short and every day is more critical than the next. India is in this phase right now. This period is all about focusing efforts in preventing transmission from the infected to those around them.
The Indian government is following a policy of ‘contact tracing’ under which it is actively trying to trace all those who may have come in contact with each infected individual.
The number of such individuals runs in hundreds. To give just two examples of the Delhi and Telangana cases, health authorities tracked down more than 150 individuals, put them in isolation and under watch, took samples of symptomatic cases and put many under quarantine at home. The teams usually work under the guidance of epidemiologists and carry out this tiring but critical job.
“All teams are briefed on who to trace and which contact should take priority. This requires an army of people. In India, we have enough workforce for this. Our institute alone has trained hundreds of people in epidemiology. There are teams at central, state and local level. NGOs can also be roped in. The contract tracing teams need to be given simple guidelines which they have to follow. That’s it. We can scale and form as many teams as we need depending on the situation,” says Dr R Prabhu at the Chennai’s National Institute of Epidemiology.
Unfortunately, six relatives of the Delhi case tested positive in Agra who he had gone to meet. This necessitated not just contact tracing but also ‘cluster management strategy’.
The government implements this whenever a large number of cases are detected at one location. An area of radius of 3 kilometres is made into a cluster and all the homes and public places are regularly disinfected while residents are kept under watch for any signs of Covid-19.
The idea is to limit the spread and block transmission to other areas. This is being done in Agra where the six cases were detected.
The authorities are also doing fumigation of the premises — like homes, schools, hotels, office buildings — visited by the infected. Covid-19 virus is highly contagious and experts say that it can remain ‘live’ at room temperature for as many as nine days and can infect anyone who comes in contact with it. That’s why any premise visited by the patient has to be disinfected.
This second chance under which the government implements aggressive contact tracing and cluster management requires large numbers of teams to track individuals and implement isolation and quarantine strategies in a small geographical area.
For instance, in China’s Wuhan, at its worst, as many as 18,000 teams of health workers, each consisting of five members including an epidemiologist, were employed round the clock in contact tracing.
The WHO study in China found that the closer one is to the infected person, the more the risk. That’s why Covid-19 patients have been found to infect their family members more than their neighbours. This helps health workers in prioritising and categorising contacts of the patient in differentiated risk categories (‘high risk contact’, ‘medium risk contact’, etc).
If the authorities are lucky enough to track all the contacts of the infected, isolate them and give proper medical care, then the spread of the disease can be contained. Success depends on both luck and the intensity of effort. Any lapses here can be more catastrophic than the lapse at the airports or ports in letting an infected patient come into the country.
Is India Prepared?
It is no news to anyone that India’s health infrastructure — both hard (hospitals, beds, equipment, etc) and soft (doctors, health workers, expertise, etc) is abysmal.
According to WHO, the number of functional hospital beds in India is 0.5 per 1,000 population, much lower than the US (2.9) and China (3.8). Number of allopathic doctors per 1,000 people in 2018 in India was less than 0.7. In the US it was 2.5 and in China 1.5.
India needs 32,900 more sub centres (SCs), 643 more primary health centres (PHCs), and 2,188 more community health centres (CHCs) to meet its basic health infrastructure requirements.
This translates into a total shortfall of 18 per cent SCs, 22 per cent PHCs and 30 per cent CHCs.
The available capacity is severely lacking in quality. In a reply to a question in Parliament, the Health Ministry said that 93 per cent of SCs and 87 per cent of PHCs and CHCs fail to meet the basic Indian public health standards (IPHS). Out of 25,743 PHCs, 63 per cent don’t even function on a 24x7 basis and the same percentage don’t have an operation theatre, over 32 per cent don’t have a labour room, and a quarter of them have less than four beds.
Rahul Gandhi has been waxing eloquent on Twitter, taunting Prime Minister Modi on his government’s preparedness regarding Covid-19. But his family and his party has to take the most blame for the aforementioned scary statistics where for decades the Congress ruled governments artificially kept the capacity of doctors limited with its license-quota raj policies.
No wonder, India is ill prepared to deal with an endemic like Covid-19. In Global Health Security Index rankings, it stood at 57 in a comprehensive assessment of global health security capabilities in 195 countries.
If there is an outbreak, the challenges that India will face is chiefly because the Congress party and Gandhi family didn’t do its job for seven decades.
Since coming to power in 2014, the Narendra Modi government has tried to ramp up capacity in healthcare. It has added 15,800 new seats in undergraduate medical courses and 7,697 in postgraduate (PG) courses in the last three years alone. (Currently, India has an intake capacity of over 80,000 MBBS seats in more than 539 medical colleges)
Intake capacity at MBBS level in colleges has been increased from 150 to 250, norms for setting up of a medical college in terms of the requirement of land, faculty, staff, bed strength and other infrastructure have been relaxed in addition to doing away with minimum land requirement for establishment of medical colleges in metropolitan cities.
The Centre is also upgrading state and central government medical colleges and increasing MBBS seats.
Additionally, it is establishing medical colleges by upgrading district/referral hospitals allowing them to start teaching operations.
Similar steps have been taken to increase seats in PG courses including raising teacher-student ratio which was kept at very low.
The government is aiming to establish 75 new medical colleges by 2023, mainly in areas which don’t have one already. Out of these, 49 have already been approved in eight different states. This will further add 7,500 more MBBS seats.
Screening, Sampling, Testing
Union Health Minister Dr Harsh Vardhan told the media in a press briefing that until 3 March, the government had screened 589,000 passengers at airports, over 15,000 at sea ports and over 10 lakh at border with Nepal. On 4 March, a universal screening of all passengers irrespective of where they are coming from was put in place and now over 30 airports have implemented it.
In addition, passengers coming from severely affected countries such as China, South Korea, Iran, Italy, etc have to undergo medical screening at ports of entry, ie, before boarding their flights.
But still a few cases which turned out to be positive managed to enter the country before these stringent measures were put in place. And they have infected many others.
Going forward, apart from containing the outbreak by contract tracing and cluster management methods, one of the biggest challenges will be having enough testing facilities in place.
The Donald Trump administration in the United States in general and the Centre for Disease Control (CDC) in particular has come under heavy criticism for faltering on this front. The CDC started sending out Covid-19 diagnostic kits in early February but they had a problem: one of the reagents was contaminated which means that it could show false positives. This blunder is now corrected.
Another problem that CDC created was that it didn’t have enough diagnostic kits to send out to labs initially and this severely impacted testing ability in the country. As cases started to pile up, the administration assured that the kits sent out to labs could now carry up to 1-1.5 million tests but there are reports of panic in hospitals and labs about availability of tests.
As of 5 March, CDC had conducted testing for only 1,583 patients (this doesn’t include testing being done at state and local public health laboratories but that began this week which means the number cannot be higher than 2,000 as one report in The Atlantic has highlighted).
Now, compare this to India. As of 6 March, a total of 4,058 samples from 3,404 individuals have been tested. This is when India has 34 confirmed cases so far (8 March) while the figure for the US has jumped to 400. A total of 52 laboratories are now active throughout India up from 10 in a matter of days. In the US, 72 labs are testing samples across 47 states.
Dr Harsh Vardhan has assured that India doesn’t lack testing capacity and laboratories can be scaled as needed and tens of thousands of tests can be carried out per day. He announced plans to take the number of laboratories capable of testing Covid-19 to more than 100 in a few days.
As far as testing is concerned, South Korea is being hailed as a pioneer with its drive-through establishments and has tested 140,000 individuals.
“Currently, the testing for Covid-19 is being coordinated by National Institute of Virology (NIV), Pune which is the apex lab. Then there are VRDLs in almost every state, most of which have already started carrying out Covid-19 tests. So, capacity is not a problem. It can be easily scaled up. All you need is to share the protocol. Right now, it’s centralised with the government labs but eventually private sector can also be roped in if the need arises,” a scientist and laboratory in charge at one of the top biomedical research institutes in the country tells Swarajya on the condition of anonymity as he is not authorised to talk to media.
“It takes less than one day (12 to 24 hours) for the results to come in. Though many labs are now conducting the tests, those who are found positive are being sent to NIV Pune for reconfirmation,” he says.
Preparation At The Lowest Level
The first meeting on Coronavirus at the highest level in the government was held by the Prime Minister’s Office (PMO) back on 25 January. Principal Secretary to the Prime Minister Dr P K Mishra had chaired a high level meeting to take stock of India’s preparedness.
This was five days before the first case was reported in Kerala on 30 January. Mishra was briefed by the Health Ministry on “hospital preparedness, laboratory preparedness, measures taken for the Capacity Building of the Rapid Response teams and the extensive surveillance activities undertaken by the Ministry”.
Since the case in Kerala came to light, the government authorities sprung into action. Officials till the district level started preparing themselves in case Covid-19 spreads. They had done this before, almost a decade back, when the swine flu pandemic shook the world including India. Between May 2009 and December 2010, 2,744 people died.
Those old files and protocols were dusted off and updated in light of Covid-19 threat.
“Sensitisation meetings of IMA members in the district were conducted in the first week of February. Hospital staff were briefed and advertisements were placed in public places and media to inform the public about Coronavirus. All the hospitals — both private and public — have been asked to create isolation wards for potential patients,” Dr Ranbir Singh, deputy Chief Medical Officer at General Hospital Jhajjar, tells Swarajya.
“We have prepared a list of logistics — number of available beds in isolation wards, ventilators, Personal Protection Equipment (PPE — gloves, N-95 masks, gowns, etc) and so on. Rapid response team has been formed for the district comprising specialist doctors as well as officials from the local and state government. In every hospital, one person has been designated as nodal officer for Covid-19 patients,” he adds.
To give a perspective about the capacity to readers, in Jhajjar district, the administration had identified 10 isolation centres (seven private, three government) where 39 beds are available in isolation wards. Thirteen beds are available in ICUs and there are 17 ventilators (nine portable, eight static) in the whole district.
Clearly, these are not enough in case of an outbreak but extra resources can be pulled from less affected areas to those which are facing a crisis.
All local authorities at the district level have been making such preparations at their own level since the past one month.
Role Of Private Sector
Whether it is the availability of beds, staff or critical equipment like ventilators (which will be needed for more vulnerable Covid-19 patients), as the above example of Jhajjar district shows, the private sector has comparatively better facilities and in some areas much better staff strength. Those will have to be put to use if the situation worsens.
While states and district administrations are coordinating with private hospitals at their level, Dr Harsh Vardhan on Tuesday (5 March) chaired a high level meeting with owners and heads of private hospitals of the National Capital Region.
Various issues related to “preparedness in terms of bed capacity of hospitals for infected cases, isolation wards, protocols for sample collection and testing, protocols for outdoor patients etc” were discussed and the minister talked of pooling collective resources to combat the emerging threat of Covid-19.
But many questions remain. Currently, all the private hospitals and even government hospitals are asked to send all Covid-19 patients compulsorily to designated nodal government hospitals for treatment.
“When the first case was reported in Delhi, the patient was sent to Ram Manohar Lohia Hospital. That was made the nodal hospital for all Covid-19 patients. Though we have dedicated swine flu isolation wards, we have been instructed to report suspect cases to the higher authorities. Then the patient is transferred to RML for his sampling, quarantine and treatment,” a doctor at Delhi’s Lady Hardinge Medical College tells Swarajya.
“Only place where samples are being taken is Kasturba Hospital in Mumbai. So, if any patient who is suspected of Covid-19 comes to us or any other hospital, he has to be sent to Kasturba Hospital where testing will be done. Currently, the government regulations do not permit the private hospitals to admit Covid-19 patients,” says Dr Laxman Jessani, an infectious disease and control specialist at Apollo hospital (Navi Mumbai).
Now that the cases have increased, other government hospitals have also been roped in for quarantining and treating patients. They are what can be called the first line of defence.
But what if the situation worsens and the government hospitals are overwhelmed? In that case, services of private sector will have to be enrolled.
Thus, it is important for the government to sort out the cost dynamics: how will the private sector be reimbursed? Will they be asked to take it on the chin or will the burden fall on patients who may not have insurance?
In such a scenario, the importance of Prime Minister Jan Aarogya Yojana (PMJAY) — Ayushman Bharat will be understood. Over 10 crore uninsured families now have insurance and will not have to bear the costs themselves.
“For PMJAY patients, there is already a sort of package that can cover hospitalisation. It is generic for things like enteric fever. There is also a provision for unspecified package. So, essentially, all the Ayushman Bharat beneficiaries should be able to get the treatment free of cost for Covid-19,” an official working in the National Health Authority tells Swarajya on the condition of anonymity as he isn’t authorised to talk to the media.
The Insurance Regulatory and Development Authority of India (IRDAI) has also asked insurance companies to come up with policies to cover treatment cost for coronavirus infection. "Where hospitalisation is covered in a product, insurers shall ensure that the cases related to coronavirus disease (COVID-19) shall be expeditiously handled,” IRDAI has said.
Additionally, the government can take care of treatment costs of every uninsured Covid-19 patient in the country as a one-time relief.
Does India Have The State Capacity?
In times of epidemics, poor, democratic countries are severely handicapped to deal with crisis. India is in that position. Its health infrastructure is not equipped to deal with a major pandemic where there is a sudden influx of patients to its already overburdened hospitals. Nor can it afford to be ruthless like the Chinese. But to repeat the done-to-death cliche “desperate times call for desperate measures’.
And thank the heavens that the Indian Constitution allows the government of the day to be tough in times of emergencies.
“All fundamental rights enshrined in the Indian Constitution are subject to morality, public order and health,” Supreme Court lawyer J Sai Deepak tells Swarajya.
If the coronavirus outbreak gets out of control, then the government can very much limit civil liberties, wall off cities, quarantine large areas by putting them under curfew, restrain the sick and isolate them from their families along with those who have had contact with the infected, and close down establishments (private as well as public) and shut down all modes of transportation for as long as the situation warrants.
Therefore, the right question is not whether the state is legally allowed to implement tough measures but if it’s capable of doing so.
If it comes to putting curfews in large parts of a state or country, the government will have to think of other aspects as well. The quarantined population in the walled off areas will need supply of food and medicines among other things. With no transportation, the government will have to do the heavy lifting.
In Wuhan, hundreds of thousands of its residents relied on food delivery apps to get their food daily. While, major cities in India where online food delivery is in place, can cope with quarantine easily, in small towns or villages, this will be difficult.
The cities or major clusters suffering from outbreak will need to be disinfected constantly. Do our municipalities have resources and manpower to do that? Thanks to the Swachh Bharat Mission, Indian municipalities are in a far better position today than they were five years ago.
Not all Covid-19 patients are serious. But those who are above 60 years of age or already suffer from ailments like blood pressure, cholesterol, diabetes are at higher risk of developing serious respiratory problems. They may need ventilator support but Indian hospitals don’t have enough to spare for Covid-19 patients.
Rural areas and poorer states are at much higher disadvantage and thus at greater risk if there is an outbreak. The central government has to be ready to shift thousands of government health workers from one state to another (or from one district to another within a state) if the situation goes south in one particular cluster (like it did in Wuhan).
The New York Times reported that in an extreme situation, some hospitals in the US are devising rationing policies which involve “removing some patients from ventilators without requiring their consent to make way for others presumed to have a better chance of survival”.
During peak epidemic, Indian hospitals filled to their capacity could refuse hospitalisation for non-Covid-19 patients if their condition isn’t critical but they don’t seem to be contemplating such rationing policies.
“Those patients who are put on ventilators are already in a serious condition so there is no question of removing them from that support. That is not an option. New patients will have to be given spare ventilators. Those in the private hospitals can be leveraged if there aren’t enough in government ones,” says Dr Jessani.
Managing Schools And Workplaces
On top of all these is the concern of closing down schools and workplaces.
In Noida, a school was closed recently because children of the Delhi patient who tested positive on 2 March studied there and was present at a birthday party attended by several kids. Thankfully, none of them got infected.
The WHO-China joint report on Covid-19 shows that disease in children appears to be relatively rare and mild with “approximately 2.4% of the total reported cases reported amongst individuals aged under 19 years. A very small proportion of those aged under 19 years have developed severe (2.5%) or critical disease (0.2%)” and importantly the WHO team didn’t come across any case where transmission took place from a child to an adult.
Nonetheless, when it comes to children, there is no taking risk. If the disease spreads, schools will have to be closed down so they have to prepare for that. Given that, most of the schools in India remain closed during peak summers and academic activity picks up pace only in July, shutting schools until then won’t have much impact on studies.
It’s the closing of workplaces which should worry India more as the economy is already in a tough spot. Paytm closed its Gurgaon office for 15 days when one of its employees tested positive recently.
Similar step was taken by a company in Hyderabad whose entire premises had to be emptied and disinfected. One hopes that the situation is contained at the earliest in India but it wouldn’t be a bad idea for companies to already start preparing for the worst and putting in place plans to have its employees work from home.
Not just schools and offices, it’s critical that hospitals also go online. That’s what China did. “First, they moved 50 percent of all medical care online so people didn’t come in. Have you ever tried to reach your doctor on Friday night? Instead, you contacted one online. If you needed prescriptions like insulin or heart medications, they could prescribe and deliver it,” says Dr Bruce Aylward, head of the WHO team which visited China.
There are reports that Delhiites are panicking when there have been only 39 cases in the country.
In Wuhan, the epicentre of Covid-19, one can only imagine the paranoia.
So, China started whipping these suspects through CT scans.
“Each machine did maybe 200 a day. Five, 10 minutes a scan. Maybe even partial scans. A typical hospital in the West does one or two an hour. And not X-rays; they could come up normal, but a CT would show the “ground-glass opacities” they were looking for (lung abnormalities seen in coronavirus patients),” says Dr Aylward.
Dr Aylaward says that from detecting symptoms to hospitalisation, China took 15 days initially which came down to two. In India, our starting point is two days which means the infected infects much smaller numbers of people and contact tracing and transmission becomes harder and the disease control becomes that much easier.
Seeing how even the developed nations like the US, Italy and South Korea are fumbling in containing the Covid-19 spread, India’s actions so far have been satisfactory except for a few missteps at airports. Most of its cases so far are imports. Community transmission is low. And the testing capacity seems to be expanding really fast without much of a hassle.
Can India pull off a miracle? One can only hope for the best.
Introducing ElectionsHQ + 50 Ground Reports Project
The 2024 elections might seem easy to guess, but there are some important questions that shouldn't be missed.
Do freebies still sway voters? Do people prioritise infrastructure when voting? How will Punjab vote?
The answers to these questions provide great insights into where we, as a country, are headed in the years to come.
Swarajya is starting a project with an aim to do 50 solid ground stories and a smart commentary service on WhatsApp, a one-of-a-kind. We'd love your support during this election season.
Click below to contribute.
Latest