Politics
Universal Healthcare In Assam: Despite Challenges, There’s Reason For Optimism
- Assam has historically grappled with several challenges in the area of healthcare policy and reform.
- Yet, despite difficulties, there are reasons to be optimistic about progress of universal health coverage in the state, as the authors of this piece argue.
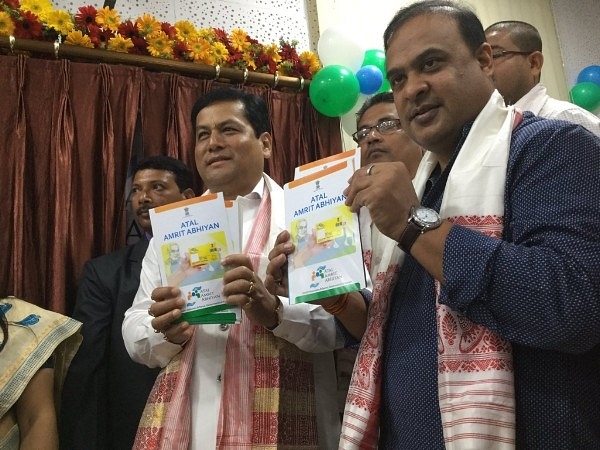
Assam Chief Minister Sarbananda Sonowal and Minister Himanta Biswa Sarma at the launch of Atal Amrit Abhiyan, a health assurance scheme for the poor. (Himanta Biswa Sarma/Twitter)
Universal healthcare, or coverage, refers to a system that provides healthcare and financial protection to all citizens of a particular country or state.
The World Health Organization (WHO) defines universal coverage as one which embodies three key principles:
1. Equity in access to health services – everyone who needs services should get them, not only those who can pay for them;
2. The quality of health services should be good enough to improve the health of those receiving services; and
3. People should be protected against financial risk.
The idea of a state or the ruling dispensation looking after the health and well-being of its citizens is not new. Many European countries have been pioneers of this concept in the modern world, either in the form of health insurance, like in France, or a system funded by tax revenue, like the National Health Service in the United Kingdom.
The first national social health insurance was developed in Germany. Under Otto von Bismarck's leadership in 1883, the German government took a fundamental step towards greater social protection in health. The British National Health Service (NHS) was founded in 1948, designed to offer majority of healthcare services to any resident free of cost at the point of delivery. Variations of this tax-funded model were implemented in Canada, Australia and New Zealand. Although the United States has historically been opposed to generalised state funding of healthcare, the provision of benefits for the elderly and the poor with Medicare and Medicaid in the 1960s and the insurance mandate through the Patient Protection and Affordable Care Act of 2010 (Obamacare) suggest the country's path.
Among low-income groups, Thailand is an example of a country that has vastly improved coverage and protection against the financial risks of ill health. It has done this by changing the way it raises funds for health and moving away from direct payments, such as user fees. Mexico and Turkey are two other examples.
Health services cost money. One way or another, doctors and nurses, medicines and hospitals are expensive. With the burden of communicable diseases still high in many parts of the world, and the increasing prevalence of non-communicable diseases – heart disease, cancers and chronic conditions such as obesity – health costs only continue to rise. This trend has been exacerbated by the more expensive and sophisticated medicines and technology being developed to treat them. Thus, to achieve universal health coverage, countries need innovative financing and operating models.
In India, a country with limited financial resources, large population numbers and a low tax base, the concept of universal coverage and its execution have challenged policy-makers and health experts for long. Moreover, when it comes to access and utilisation of healthcare services, the country is divided; those who live in the urban areas of India have access to medical care, albeit expensive and of varying quality. However, the majority of India lives below the poverty line in rural areas and has extremely limited access to medical care. High out-of-pocket expenditure is a concern for Indians and it currently stands at approximately 71 per cent.
The country has made some tentative progress towards providing a security net for healthcare expenses, Employee’s State Insurance Scheme (1948), Central Government Health Scheme (1954) and Rashtriya Swasthya Bima Yojana (2009), among others.
The National Health Policy, 2017, announced universal health coverage as its core objective with the aim of delivering quality healthcare services at affordable costs to all. The policy proposes an incremental assurance-based approach to tackle the issue of coverage and access. It proposes a health card for every family, which will enable access to primary care facilities and a defined package of services nationwide. Drugs, diagnostics and emergency care services are to be offered free of cost in all government hospitals.
Incidentally, the new policy also aims to increase public spending on health to 2.5 per cent of the gross domestic product (GDP) by 2025. Right now, India spends a meagre 1.15 per cent of its GDP on health – well below the WHO recommendation of 5 per cent.
Healthcare status in Assam
Assam’s population of 3.25 crore (approximately) has suffered due to piecemeal development of its healthcare infrastructure. Assam has a diverse geography of char areas (flood plains; approximately 10 per cent of the population), tea garden areas (approximately 20 per cent), hill districts and forest areas. The challenges to healthcare delivery range from accessibility to manpower deployment but also, more importantly, socio-cultural. Hence, a pattern has emerged of variable penetration of healthcare services and schemes linked to geography of the state. Assam is a consistent worst performer in Maternal Mortality Ratio, Infant Mortality Ratio and under-five mortality rates, which is a cause of shame.
Assam’s vulnerability to annual floods and resultant communicable disease spectrum is a healthcare provider’s nightmare. Although only 14 per cent of the population live in urban areas, non-communicable diseases are creeping in aggressively. Assam boasts one of the highest rates of cancer, hypertension and diabetes in the country.
Status of healthcare coverage in Assam
The National Family Health Survey (2015-16) revealed only 10.4 per cent of the households have at least one member covered under any health scheme. This makes Assam the third-lowest ranking state in India in this regard. The reasons for this low coverage are many – large-scale migration, especially of the head of the family who is unavailable for enrolling and availing of such schemes, lack of awareness both of “rights” as well as availability and accessibility; behaviours and cultural practices in different pockets of the state also contribute.
A quick look at the past decade shows the launch of a number of schemes aimed at improving coverage and accessibility, especially for the economically and socially disadvantaged; “Mamoni”, “Majoni”, “ Morom”, “Arogya Nidhi” and so on. The shelf lives of these schemes and successes have been variable. Operation Smile and the free Congenital Heart Disease Treatment Scheme are perhaps two of the only successful schemes that have been sustained through the recent years.
Current scenario
In 2016, soon after the present government came to power, it announced the launch of Atal Amrit Abhiyan – a health assurance scheme covering 438 critical care procedures in the six specialties of cardiac disease, cancer, neurology, kidney disease, neonatology and burns. It is the largest individual-based health assurance scheme in the country which aims to cover approximately 92 per cent of the population of Assam. It is cashless and card-based, and assures every eligible individual with an annual family income of below Rs 5 lakh a sum of Rs 2 lakh per annum.
The scheme can be availed of in empanelled hospitals within the state and in selected cities of India. It could potentially be a game-changer and bridge the following key gaps:
(a) Access to quality tertiary care for majority of Assam’s population
(b) Access to high-cost care
(c) Improve health outcomes and quality of life for much of Assam’s population suffering from chronic and critical care conditions
Free diagnostics: The recently announced Chief Minister’s free diagnostics services is envisaged to ensure availability of a set of diagnostics services at health institutions with CT scan, X-ray and laboratory services provided free of cost to all, irrespective of whether anyone is from Above the Poverty Line (APL) or Below the Poverty Line (BPL).
Mobile medical units for tea gardens: Some of the lowest health outcomes and provisions are seen in Assam’s tea gardens. Under this scheme, two mobile vans (a MMU unit) equipped with laboratory diagnostic facilities and a minimum number of key health personnel will visit individual tea gardens and station themselves for a week in each; thus, in a week 80 tea gardens and, in a month, 320 tea gardens shall be visited by the 80 MMUs currently being commissioned.
Ramping up the services of boat clinics in char areas, an ambitious programme of commissioning new health infrastructure, are all well-intentioned schemes that have been recently launched. The government has also declared its intentions to re-contour the employees health benefits scheme to make it more accessible and in tune with today’s times.
Challenges
Implementation has been confirmed as the most important aspect in any health sector policy reform, none more than improving quality, access and coverage. Difficulties have been reported in Assam historically, which reflected inadequate planning of implementation, be they with the timing, governance, infrastructure (including information systems and manpower), participation of stakeholders and, very importantly, the financial resources needed.
Thus, the same degree of thought and effort that goes into developing policies should also go into developing an implementation strategy and in monitoring the entire lifecycle of the scheme. Despite these challenges, our conclusion is that there are reasons to be optimistic about progress of universal health coverage in Assam as there seems to be: (i) political will (ii) ring-fenced resources (iii) an outline strategy for upgrading of infrastructure and skills.
Introducing ElectionsHQ + 50 Ground Reports Project
The 2024 elections might seem easy to guess, but there are some important questions that shouldn't be missed.
Do freebies still sway voters? Do people prioritise infrastructure when voting? How will Punjab vote?
The answers to these questions provide great insights into where we, as a country, are headed in the years to come.
Swarajya is starting a project with an aim to do 50 solid ground stories and a smart commentary service on WhatsApp, a one-of-a-kind. We'd love your support during this election season.
Click below to contribute.
Latest