Ideas
Five Reasons Why ‘National Health Policy 2017’ Is A Step In The Right Direction
Ananya Awasthi
Mar 23, 2017, 10:58 AM | Updated 10:58 AM IST
Save & read from anywhere!
Bookmark stories for easy access on any device or the Swarajya app.


As we analyse the Indian policy discourse, we find that healthcare financing and service delivery continues to stand out as an exception. Not only does it remain to be one of the least understood sectors but also, probably, is the worst performing amongst all.
Even after 70 years of Independence, 45,000 mothers die each year during childbirth (highest in the world), 43.5 per cent of children under the age of five are underweight and malnourished (higher than Sub-Saharan Africa), and every year around 2,20,000 people lose their lives due to tuberculosis (highest burden in the world).

Also, quite contrary to the Western perception - the three biggest killers in India are not infectious diseases but are, in fact, non-communicable diseases like heart disease (12 lakh deaths annually), lung disease (10 lakh deaths annually) and stroke (9 lakh deaths).
As a result of which, India’s healthcare indicators are not only worse than all the other BRICS countries and those with comparable growth statistics but are also lagging behind its neighbours like Bangladesh, Bhutan and Sri Lanka.
Health care crisis continues to exist despite the fact that over all these years, tax payer’s money has been continuously pumped to finance ad-hoc vertical schemes and piecemeal expansions of the fractured public health systems. Here it is important to note that healthcare spending in India (1 per cent of GDP) is also one of the lowest in the world.
Though the HLEG group in 2012 did recommend an increase in the public health expenditure to 2.5 per cent of GDP, no action in this regard was taken by the then ruling government. Still, it will be useful to take stock of how these resources have been spent and whether the so-called ‘investments’ made in the public health sector reaped any healthcare dividends.
Using the traditional indicators of health, we have already seen how poorly India fares on all most all of them. Alternatively, let us use the lens of healthcare financing to describe the actual plight of a poor patient in India.
Do we know that despite having an overarching National Health Mission for the past 12 years (started as NRHM in 2005 by the UPA government) and the presence of the so-called socialist model of healthcare financing, the out of pocket payments (OoP) in India (67 per cent) are one of the highest in the world.
It means that if an average Indian spends Rs 100 to seek medical care, up to Rs 67 is spent by his/her own pocket and less than Rs 30 is covered by the government and other methods of health insurance. Moreover, 70 per cent of OoP is on the purchase of drugs and diagnostics.
What is particularly disheartening is that every year about 6 crore Indian households fall below the poverty line due to catastrophic healthcare expenditures. And the majority of this financial burden falls on the underprivileged members of the society like the Dalits, tribals, rural and poor households.
Not surprisingly as high as 86 per cent of rural population and 82 per cent of urban population are still not covered under any scheme of health expenditure support/insurance system.
The Central Government, however, recently has brought over 12 per cent urban and 13 per cent of rural population under some form of health protection coverage like the Rastriya Swasthya Bima Yojana.
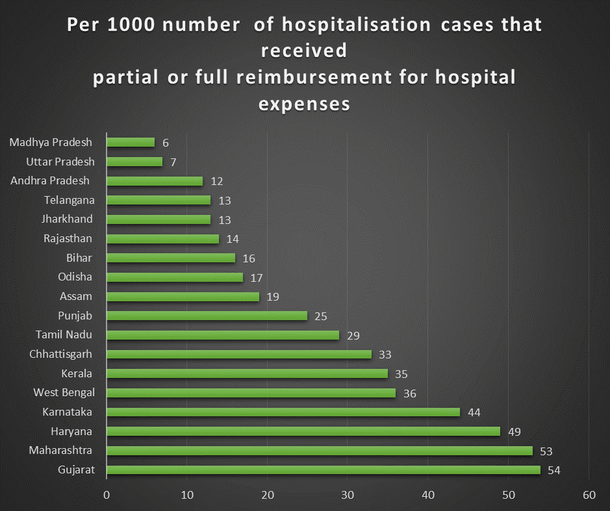
What is interesting to note is the large inter-state variation in the financial protection for healthcare provided by various states. The following data from the National Sample Survey Organisation (NSSO) 71st round reveals that states with the highest percentage of reimbursement of hospitaliastion expenses were Gujarat, followed by Maharashtra and Haryana, thus providing the best safety net against catastrophic healthcare spending.
Whereas Kerala, Karnataka and Chhattisgarh had only 2 per cent of their cases reimbursed for hospital expenses, and the other states fared even lower.
Yet the public narrative for health sector has remained unchanged since independence, focussing on merely inventing newer public programmes without imposing any incentive for improving either accountability or efficiency of healthcare delivery in the public sector.
Misguided by the dominant discourse of development economics and statist model for public health in India, current situation of district hospitals and health centres is marked by doctor absenteeism, drug stock outs and rampant corruption, all leading to delays in access, quality and accountability of healthcare.
Ultimately a poor rural Indian is left with only two choices:
One: Use a public health centre which offers poor quality of services.
Two: Go to a private hospital and access expensive care in the absence of any universal health coverage.
In light of the above, it becomes very pertinent for policy experts to analyse if we can afford to ignore the private sector and the choices people make while accessing health care.
According to government’s own NSSO estimates (71st round) nearly 70 per cent of the total health ailments in India are being treated at private facilities. To be even more precise, the same data shows that as much as 75 per cent of outpatient (OPD) care is exclusively private and more than 55 per cent of inpatient (IPD) care is sought from private hospitals in India.
Hence, it is rather surprising to see why and how the public discourse on healthcare has until now remained oblivious of the presence of private sector in healthcare.
Any narrative on Public-Private Partnership has been unfairly made out to be a shift towards abolition of public health systems and leaving the general population at the mercy of an unregulated and costly private sector - which is, in fact, far from the truth.
Hence an informed debate about the need for health insurance leading to universal health coverage never penetrated the public discourse, until the draft of the new National Health Policy 2017 was shared with the public for inviting suggestions two years ago.
After taking due consideration of the suggestions received, the health minister came out with the final recommendations of the policy. Let us see how this new health policy affects us and whether it fits into the healthcare needs of an average Indian.
First, the policy rightfully signals the coming of a health insurance era in India, leading to universal health coverage. Some analysts have gone to the extent of labelling these reforms as the Obamacare. India version!
This policy direction is also in alignment with the recommendations of the World Health Organisation which calls upon all the countries to adopt a health insurance model, thus providing universal health coverage against an essential package of primary, secondary, and tertiary services.
It will provide healthcare access to millions of poor households, reduce poverty arising out of catastrophic spending on healthcare and promote a significant reduction of out of pocket expenses, which in some cases, can mean the entire life savings of a BPL (below poverty line) household.
This is in contrast to the present scenario where only a handful of government employees and a miniscule of the formal sector have access to any sort of health insurance.
Second, the government commits to an increase in the public health expenditure from the current 1 per cent of GDP to 2.5 per cent, which will be the biggest jump in healthcare expenditure that India will see since the Independence.
And a majority of this expenditure is geared towards making drugs and diagnostics more affordable, thus addressing a major (70 per cent) proportion of out of pocket expenses.
Now the question arises, whether the government hospitals and health centres can alone shoulder the responsibility of treating the humongous disease burden of 120 crore Indians?
As of today, private sector accounts for 93 per cent of all hospitals (up from 8 per cent in 1947), 64 per cent of all beds, and 80 to 85 per cent of all doctors. As opposed to the common understanding, this penetration of the private sector holds equally true for the rural areas where 70 per cent of all the primary care visits are also to private health care providers.
Hence, as a third logical step, the National Health Policy recommends for a mix of public and private care to ensure that every insured individual, irrespective of caste, sex or religion should have a right to choice, efficiency and quality.
Thus, if implemented, a poor rural household won’t be forced to use poor quality of public health services only because of his inability to pay. Instead, the public facility would be incentivised to improve the quality of service delivery in the face of competition and efficiency from the private sector.
This however needs to be accompanied by proper regulation of the quality of care that even the private sector is providing.
Fourth, the need for focusing on non-communicable diseases like diabetes, heart and lung diseases, which have a lion’s share in India’s disease burden, has been rightly recognised, thus making for the most efficient use of the resources.
Finally, the policy gives a big push to health research as an important means for building evidence base for public health in India.
Though implementation remains to be seen, the new National Health Policy 2017 is a step in the right direction.
Moreover, this change in the public health narrative is also in alignment with the recommendations by the WHO, World Bank and the best practices worldwide, while being grounded to the contextual realities of the country.
Hence from a human rights perspective, it can be safely concluded that the proposed universal health coverage via health insurance with the right mix of public and private providers can soon fulfil the dream of seeking healthcare as a matter of fundamental right for every Indian.
This will especially touch the lives of poor and rural households, women, tribal and all the other socially weaker sections of the society; further fulfilling the directive principles of equitable distribution of wealth and resources across the citizens and the Vedanta Philosophy of “Sarve Santu Niramaya” (Let no one be ill).
Dr. Ananya Awasthi is a Masters in Global Health from Harvard University and writes on Public Health, Wellbeing and Indic Philosophies.