Ideas
India’s Public Health System Needs To Write Out A Prescription For Preventive Care
Urvashi Prasad
Dec 15, 2017, 06:44 PM | Updated 06:43 PM IST
Save & read from anywhere!
Bookmark stories for easy access on any device or the Swarajya app.


The India State-Level Disease Burden report released last month is the first effort of its kind to provide comprehensive risk factor and disease trends for every state in the country. The findings are a mixed bag.
Although we have reduced the burden of disease attributable to conditions like diarrhoea, tuberculosis and lower respiratory infections, the numbers still remain high. At the same time, illness and premature deaths due to non-communicable diseases like heart ailments, stroke and diabetes are rising at an alarming rate.
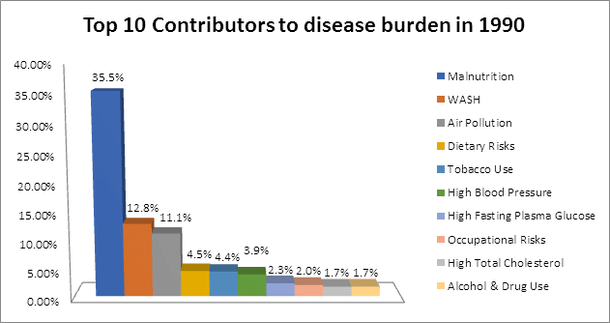
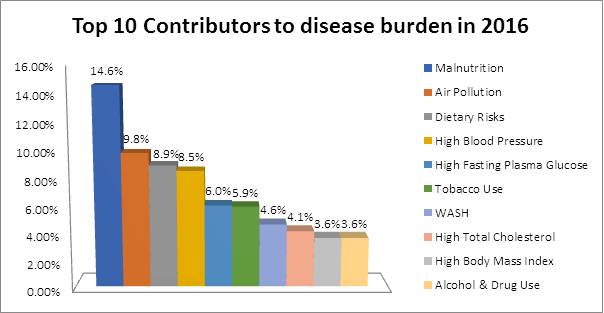
With respect to risk factors too, the report is a harbinger of both good and bad news. While we have made significant progress in the area of water and sanitation, the work is far from over. We also continue to have a very high prevalence of maternal and child malnutrition. The contribution of risk factors like high blood pressure, tobacco use and high body mass index to the total disease burden is increasing, thereby explaining the rising incidence of non-communicable diseases. All of this is exacerbated by the large disparities in outcomes between states.
The report has several implications for policy, but here are five areas that should be prioritised.
First, never before has the proverb “prevention is better than cure” been more relevant for India. Seven-year-old Adya, who has been in the news lately for losing her battle with dengue at Gurgaon’s Fortis Hospital, might never have needed a hospital in the first place if we had systematic measures in place for preventing mosquito breeding. Historically, we have had a strong bias towards curative rather than preventive care. For a country facing a dual burden of disease (communicable and non-communicable), this approach is simply untenable. It is imperative therefore that the government invests in setting up a strong public health system.
A large part of the government’s expenditure on health should focus on targeting important risk factors for disease, like high blood pressure and smoking. Preventive health messages must emphasise our traditional systems of well-being like yoga.
Another critical aspect is screening the population for early symptoms so that treatment can be initiated promptly and people can be kept out of already overcrowded hospitals.
As highlighted in NITI Aayog’s Three-Year Action Agenda, perhaps the single most important step for injecting life into our public health system is the creation of a designated focal point within the Health Ministry. Health has many determinants including nutrition, drinking water and sanitation. Coordinating with multiple ministries and pinning down accountability are a constant challenge.
A single entity with adequate authority and resources should therefore be tasked with performing the functions of educating citizens, monitoring health status and enforcing public health regulation. A state-level counterpart to the public health focal point in the Health Ministry would also need to be established.
Second, we must prioritise the delivery of a comprehensive package of primary healthcare services, including early detection and referral of non-communicable diseases. Thus far, primary care in India has been focused on reproductive and child health. A majority of illnesses can be tackled at the primary care level before they become more complicated and expensive to treat. The United States is a case in point, where a staggering 60 per cent of the total spending on health is incurred on 1 per cent of people who are admitted in tertiary hospitals.
Third, a system for generating credible data on risk factors and health outcomes at regular intervals must be established urgently. To be most useful for policy-making, this data should be disaggregated to the level of districts. Understanding the health of India’s states is useful, but for a country as large and diverse as ours, regular data on the health of the nation’s districts would be more directly actionable.
Fourth, there is an urgent need to strengthen the human resources backbone of our health system through the development of a comprehensive policy covering staff recruitment, performance management and incentives for serving in difficult areas. The institutions governing medical education also need systematic reform. The National Medical Commission Bill 2016 should be enacted and implemented as a priority, followed by a revamping of the nursing, dentistry and pharmacy councils.
Further, we need to step up efforts to expand our excessively doctor-dependent system to also include non-physicians who are trained in primary, community and family medicine.
Fifth, as emphasised in the National Health Policy 2017, we will not achieve the desired outcomes if we do not address the social determinants of health effectively. The approval of the National Nutrition Mission by the union cabinet earlier this month is a major step forward. The mission will have representatives from all relevant ministries to facilitate the much-needed programmatic and geographic convergence. As far as water and sanitation are concerned, the commendable progress we are making on providing access to infrastructure needs to be complemented with an equally strong focus on ensuring the functionality and usage of facilities. Promoting critical hygiene behaviours such as hand-washing with soap must also be high on the agenda.
It is well-known that India has one of the lowest levels of public spending on health. However, as we advocate for an increase in the health budgets, we must also have a clear plan for how we will spend the additional money. When Bill Gates was in India last month, he highlighted that the US spends 18 per cent of its gross domestic product (GDP) on healthcare and no one else even comes close. Unfortunately though, the US is perhaps not the best example for India to emulate. Despite spending such a large sum on health, the life expectancy in the US is around 78.7 years, which places it twenty-seventh among OECD (the Organisation for Economic Co-operation and Development) members. By defining our priorities as outlined here, we can ensure that we get more health for the money we spend.
Disclaimer: The views and analysis expressed in the article are personally those of the author.
Director, Development Monitoring and Evaluation Office, NITI Aayog.