Ideas
Rajasthan’s Bhamashah Swasthya Bima Yojana: A Lack Of Awareness Is The Sticking Point Of The Project
Swati Kamal
Mar 12, 2018, 02:28 PM | Updated 02:28 PM IST
Save & read from anywhere!
Bookmark stories for easy access on any device or the Swarajya app.

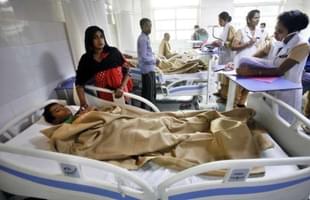
The Bhamashah Swasthya Bima Yojana (BSBY) is Rajasthan’s flagship healthcare scheme that provides hassle-free, quality healthcare to all National Food Security Scheme (NFSS) families.
BSBY is one part of the complete Bhamashah scheme. The name comes from history: Bhamashahwas Maharana Pratap’s financier, a person of immense integrity and courage. But apart from the imposing name, the envisioning of the scheme is also grand: the Bhamashah scheme in totality is a digitisation programme. It is the first household-level identity scheme to create a comprehensive dataset with the objectives of financial inclusion, women’s empowerment, by designating women as head (mukhiya) of the family, and effective government service delivery (direct transfers and non-cash benefits).
The insurance part of the scheme is generous and has a larger cover for critical care compared to other states at Rs 3 lakh. It also has a larger scope, covering secondary healthcare also apart from tertiary care.
The Scheme
Like all other health insurance schemes, the basic aim was to reduce out-of-pocket expenses in times of illness to the poor and provide them financial security. In addition, the idea was also to create a wide health database, which would help policy decisions later. But most importantly, the scheme was envisaged as being the instrument by which to bring about a revolution in healthcare in the rural areas, as the private sector would be encouraged to open hospitals in rural areas, thereby reducing the burden on government facilities. As of January this year, close to 14 lakh people have been helped by the scheme according to government estimates. The total number of health conditions covered is 1,715.
Informal estimates put the number of beneficiaries at 4.5 crore, or 67 per cent of the population. The beneficiaries were those enrolled in the National Food Security Act (NFSA) and RSBY (Rashtriya Swasthya Bima Yojana), until the Bhamashah cards were issued. To avail BSBY, beneficiaries must not only be eligible under NFSS but should also have taken rations at least once in the three months prior to the hospitalisation.
The process is as follows:
* The beneficiary has to give his Bhamashah ID and an ID proof (hospitals prefer Aadhaar over other IDs because insurance companies prefer Aadhaar verification).
* He/she goes to an enrolled hospital.
* A Swasthya Sahayak (health helper) in the hospital checks if the beneficiary is covered under NFSA, if the beneficiary has taken ration from an fair price shop dealer in the past three months. If yes, the Swasthya Sahayak verifies the beneficiary through Aadhaar by biometric authentication.
* Beneficiaries can now receive free treatment if their treatment requires hospitalisation for more than 24 hours. After the treatment, the beneficiary is required to fill out the feedback form. One copy of the feedback form remains with the hospital, which is uploaded to the Bhamashah portal. The form details the treatment, total expenditure, and total balance left under BSBY and comments from the patient.
A distinguishing factor from schemes in other states was the inclusion of secondary care, apart from tertiary care. Thus, insurance cover of Rs 30,000 for general illness and Rs 3 lakh for critical illness was to be given to families. Also, pre and post hospitalisations and transport were thoughtfully covered. The number of illnesses covered was the largest in the country to date, at 1,715, with around 170 being reserved for government hospitals. If a medical facility was unavailable in a hospital, the hospital management was responsible to ensure that they contract such facilities - the patient’s health and finances being the primary concerns. The benefits to patients are cashless and available through 475 public health facilities and 568 empanelled private hospitals across the state.
The state went for the insurance agency model, with the public-sector company, The New India Assurance Company, roped in after a bidding process. In fact, they removed the concept of a third party administrator in order to reduce costs.
Evaluation Of The Scheme
Is it a bid to please the private healthcare sector?
Just as the scheme was launched in 2015, the Economic and Political Weekly carried an article titled, “Privatising Healthcare in Rajasthan” by Narendra Gupta and Chhaya Pachauli of the Prayas Centre for Health Equity and Jan Swasthya Abhiyan (Rajasthan). This study alleged that the proposed insurance scheme was the result of lobbying by several corporate hospitals – in order to corner public health funds. This did seem plausible given that it came alongside another major measure taken by the Rajasthan government to hand over 300 public health centres (PHCs) to private operators – under the “Run a PHC Scheme” – through the process of bidding. Contrary to the original intent of offering only those PHCs that were in far-flung areas, it was found that in reality most were around urban centres and had easy accessibility; this later fact would make it easy for private facilities to make these PHCs their satellite centres for getting patients to their hospitals. The authors concluded that “It seems that finally all segments of public health system – primary, secondary and tertiary are being thrown open to the predatory private medical sector in Rajasthan”.
As per a paper uploaded on phmindia (People’s Health Movement – India/Jan Swasthya Abhiyan or JSA), there were several inefficiencies in the BSBY scheme that JSA was creating awareness about and holding dialogues for. Cases were cited where people had had to go through several hardships in availing the scheme because of the complicated eligibility criteria, and how they were being misled by private healthcare centres to cough up funds despite the insurance cover. They also highlighted the poor quality of services being delivered, and the lack of a mechanism to monitor that. Thus, they felt that the health facilities should be taken back by government under its full control, and infrastructure and human resources at public health facilities must be improved.
Low Awareness
The original intent apart, the scheme did benefit the people who now had access to the comfort and care of private hospitals. Earlier, they were used to receiving minimal treatment in over-crowded government hospitals; now they were delighted to receive good-quality healthcare at no cost.
However, overall the awareness about the existence of the scheme was abysmal. A joint study was carried out by Microsave and Center for Global Development in a paper titled “Household Perception and Impact of Bhamashah & Digital Governance Reforms in Rajasthan”. BSBY, it will be remembered, is one part of Bhamashah. They surveyed 633 households and found that 39 per cent beneficiaries were aware of BSBY and, as a consequence, only 4 per cent households had tried availing it. Those that had tried it were mostly satisfied; but many households are either ignorant of the scheme itself or of the process, the eligibility requirements, and even the list of treatment services that BSBY covers. Due to this, households are either denied services or illegally charged by hospital staff for scans, medicines, and other treatments. There were even cases where hospitals were not aware of BSBY providing coverage for such services. In July 2016, the Rajasthan government tried to create awareness about BSBY features and benefits. However, the results were not encouraging owing perhaps to the meager allotment of Rs 25,000 per district health committee.
Strange And Complex Eligibility Criteria
One of the strangest clauses of the scheme is its linking with NFSA eligibility, which states that beneficiaries must have taken rations in the last three months. This clause results in excluding genuine beneficiaries, as they could have other reasons for skipping taking rations from the dealer. At times, the research found, there were cases where beneficiaries had been incorrectly excluded from NFSA because of biometric failures, digitisation errors, etc, which were no fault of theirs.
Key Learnings
- The idea of secondary care as part of the insurance scheme is a first, as most other states have only tertiary care as part of insurance. This can be replicated to improve overall health.
- The integrated approach to healthcare sector through the two schemes – BSBY and the Arogya Rajasthan campaign that compiles health data of rural population in the state and provides people with e-health cards – will improve the health sector and encourage preventive health.
- Communication to increase awareness levels among beneficiaries is of paramount importance. The communication strategy should utilise text messages on phones as well as advertisements in television, radio, and newspapers, street plays, etc, whatever works for the region.
- Monitoring is important. While public-private partnerships are essential for effective service delivery, an independent mechanism to ensure quality service to review, audit, and assess these institutions and take timely recourse are essential.
- Among instances of malpractices by private facilities were false (non-existent) claims and highly inflated claims (compared to government facilities). After malpractices were found, even Chief Minister Vasundhara Raje stressed on the need for the state health department to monitor private hospitals that have been allotted land on concessional rates, to make sure they were treating below poverty line patients as per the norms.
- A grievance redressal mechanism for beneficiaries must be in place.
- Involvement of one or several rural healthcare NGOs would be beneficial in many respects.
- Documents required to avail of the scheme must be simple; a single ration or Aadhaar card should be able to trace eligible patients through the state’s health data management system. This would save the patient’s family the stress of collecting identity and other documents at critical moments in emergency situations.
- This follows from the previous learning: patients in need of emergency care should be admitted without questioning their eligibility; BSBY support staff could later help collect and produce documents.
- There should be a mechanism to connect patients to the right hospitals in time. Suppose a hospital is unable to provide treatment at that point because of non-availability of doctors or infrastructure, that hospital should be able to help the patient reach the correct healthcare facility. Hospitals must be made liable for this, and this will also check their tendency to deny treatment or services to patients.
Read parts one and two:
Lessons For Modicare From YSR’s Aarogyasri Project In Andhra Pradesh
Key Takeaways From Yeddyurappa’s Vajpayee Arogyashree Scheme For A Comprehensive Modicare
Swati Kamal is a columnist for Swarajya.